Why AI Won't Replace Radiologists: A Toronto Case Study in Human Expertise
In the rapidly evolving landscape of artificial intelligence, one profession stands out as a compelling case study for why human workers remain irreplaceable: radiology. While AI has made significant strides in medical imaging analysis, the nuanced expertise of radiologists in cities like Toronto demonstrates that technology serves as a powerful tool rather than a replacement for human judgment.
The Limitations of AI in Medical Diagnosis
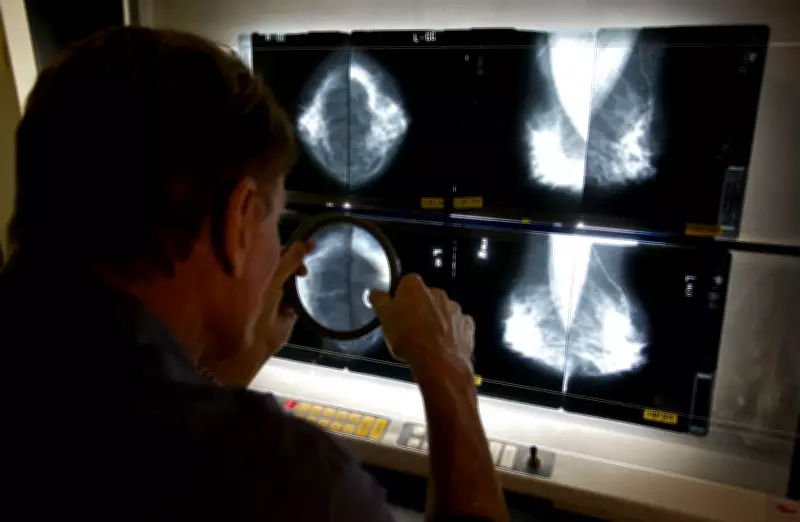
Artificial intelligence systems excel at pattern recognition and can process vast amounts of imaging data with remarkable speed. However, they lack the contextual understanding and clinical reasoning that human radiologists bring to their work. A radiologist checking mammograms doesn't just identify anomalies; they interpret findings within the broader context of a patient's medical history, symptoms, and risk factors.
This human element becomes particularly crucial in complex cases where subtle variations in imaging might indicate different conditions. AI algorithms, while increasingly sophisticated, still struggle with the gray areas that require clinical experience and intuition. The technology can flag potential issues, but determining their significance often requires human expertise.
Toronto's Healthcare System as a Prime Example
In Toronto's major medical centers, radiologists work alongside AI systems to enhance diagnostic accuracy rather than being replaced by them. This collaboration represents the future of medical imaging: technology augmenting human capabilities rather than eliminating human roles. The city's healthcare institutions have implemented AI tools to help radiologists prioritize cases and identify patterns, but final diagnoses and treatment recommendations remain firmly in human hands.
This approach recognizes that medical imaging interpretation involves more than just identifying abnormalities. Radiologists must communicate findings to other healthcare providers, explain results to patients, and make recommendations based on the complete clinical picture. These interpersonal and decision-making skills remain uniquely human capabilities that AI cannot replicate.
The Evolving Role of Radiologists in the AI Era
Rather than replacing radiologists, AI is transforming their role in several important ways:
- Enhanced Efficiency: AI can handle routine screening tasks, allowing radiologists to focus on complex cases that require deeper analysis
- Improved Accuracy: When used as a second set of "eyes," AI systems can help reduce oversight and improve diagnostic precision
- Workflow Optimization: AI tools can prioritize urgent cases and streamline administrative aspects of radiology practice
- Continuing Education: Radiologists must now develop new skills to effectively collaborate with AI systems and interpret their outputs
This evolution mirrors broader trends in healthcare technology, where AI serves as a powerful assistant rather than a replacement for medical professionals. The human elements of empathy, ethical judgment, and complex decision-making remain essential components of quality patient care that technology cannot provide.
The Future of Radiology in Canada's Healthcare System
As Canada continues to integrate AI into its healthcare infrastructure, the role of radiologists will likely become more specialized rather than diminished. Medical imaging professionals will need to develop expertise in working alongside AI systems, interpreting their outputs, and making final clinical judgments. This represents a significant opportunity for professional growth and enhanced patient care rather than a threat to employment.
The Toronto case study demonstrates that successful AI implementation in healthcare requires careful consideration of how technology complements rather than replaces human expertise. As AI continues to advance, the most effective approach will likely involve collaborative systems where human judgment guides and validates technological outputs, ensuring the highest standards of patient safety and care quality.





