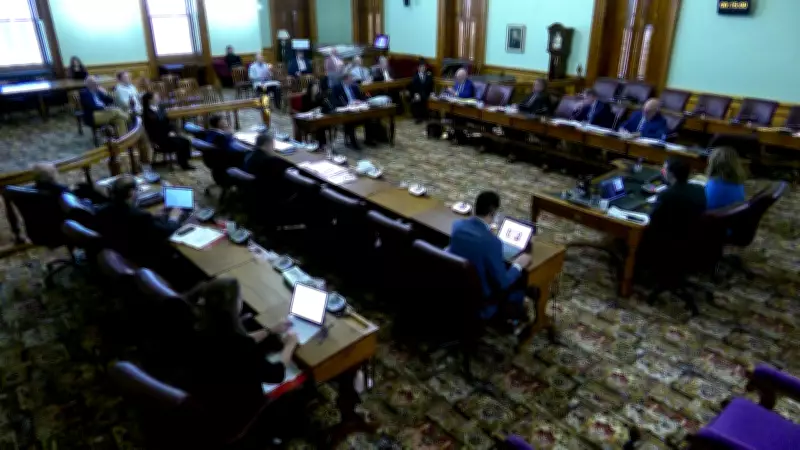
Virtual Care and Primary Access Take Center Stage in New Brunswick Health Committee
A New Brunswick legislative committee has been dominated by discussions on virtual care and primary care access, with health officials presenting detailed insights into the province's healthcare challenges. The committee, which convened recently, focused on systemic issues in healthcare delivery, highlighting both opportunities and obstacles in modernizing New Brunswick's medical services.
Expanding Virtual Healthcare Services
Health officials emphasized the growing importance of virtual care in New Brunswick, particularly for rural and remote communities. The discussions revealed plans to expand telehealth services, which have become increasingly vital for patients who face geographical barriers to in-person appointments. Officials noted that virtual care can improve access to specialists and reduce wait times for consultations, though they acknowledged the need for robust technological infrastructure and digital literacy support.
Primary Care Access Challenges
The committee also addressed persistent challenges in primary care access, including physician shortages and long wait times for family doctors. Health officials presented data showing that many New Brunswickers still lack a regular healthcare provider, leading to increased pressure on emergency departments. Strategies discussed included recruiting and retaining more healthcare professionals, optimizing clinic workflows, and integrating nurse practitioners and other allied health workers into primary care teams.
Systemic Healthcare Delivery Issues
Beyond virtual and primary care, the committee explored broader systemic issues in New Brunswick's healthcare system. Topics included:
- Resource Allocation: Ensuring equitable distribution of healthcare resources across urban and rural areas.
- Patient Outcomes: Improving health outcomes through preventive care and chronic disease management.
- Interagency Collaboration: Enhancing coordination between healthcare providers, government agencies, and community organizations.
Officials stressed that addressing these issues requires a multifaceted approach, combining policy changes, funding adjustments, and community engagement. The committee's discussions are expected to inform future healthcare initiatives in New Brunswick, with a focus on making the system more responsive to patient needs.
Looking Ahead: Policy Implications
The legislative committee's focus on virtual care and primary access reflects broader trends in Canadian healthcare, where digital innovation and access equity are becoming priorities. As New Brunswick grapples with an aging population and rising healthcare demands, the insights from this committee could shape provincial policies for years to come. Health officials committed to ongoing dialogue with stakeholders to ensure that any reforms are evidence-based and patient-centered.
The committee's work underscores the critical role of legislative oversight in healthcare governance, as New Brunswick seeks to build a more resilient and accessible medical system for all residents.