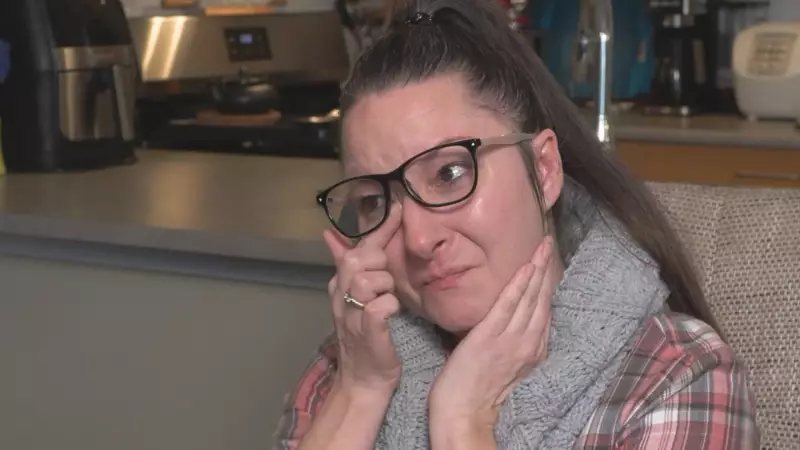
A woman in British Columbia is making a public and heartfelt plea to the provincial government, urging officials to provide coverage for a new drug used to treat multiple sclerosis (MS). Her appeal, reported on January 8, 2026, underscores the personal and financial struggles faced by patients when essential medications are not included in public health plans.
The Personal Struggle Behind the Plea
The core of this story is a direct appeal from a patient to the government of British Columbia. While the original report did not name the specific drug, the woman's situation highlights a common challenge in Canadian healthcare: access to newer, often expensive, specialty medications. Patients with chronic and complex conditions like multiple sclerosis can find themselves in a difficult position when a potentially effective treatment is available but not financially accessible through public insurance.
The Broader Context of Drug Coverage in Canada
In Canada, drug coverage is a patchwork system. While hospital and physician services are covered under the Canada Health Act, prescription medication coverage outside of hospitals falls primarily to provincial plans and private insurance. This often leads to disparities where a drug is covered in one province but not in another. The decision by B.C.'s government on whether to add a new drug to its formulary—the list of medications it pays for—involves complex evaluations of clinical evidence, cost-effectiveness, and budget impact.
For individuals with rare or debilitating diseases, the wait for a positive coverage decision can be agonizing. They may face the impossible choice of paying thousands of dollars out-of-pocket, seeking access through clinical trials, or going without a treatment that could significantly improve their quality of life. The woman's public plea brings a human face to these bureaucratic and policy challenges.
Potential Impacts and the Path Forward
Public advocacy like this can sometimes influence policy. By sharing her story, the patient aims to put pressure on policymakers to review the drug for coverage. It also raises public awareness about the gaps in Canada's pharmacare system, a topic of ongoing national debate. The outcome of her appeal could set a precedent for how B.C. handles similar requests for other high-cost therapies for neurological conditions.
The fundamental issue remains balancing finite healthcare budgets with the imperative to provide patients with the best available treatments. As medical science advances, producing more targeted but costly therapies, this tension will only increase. The call from this B.C. woman is a poignant reminder that behind every coverage decision are individuals and families hoping for a better quality of life.