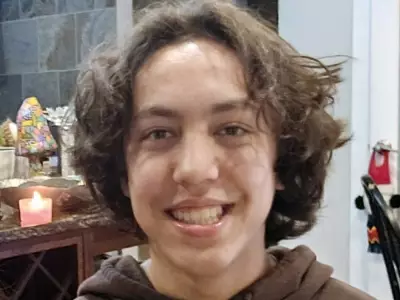
As Canada marks Alzheimer's Awareness Month, one woman's nearly two-decade journey caring for her mother casts a stark light on the profound challenges facing families navigating dementia within the nation's healthcare system. Naomi Mison has spent most of her adult life as a caregiver after her mother was diagnosed with young-onset dementia at just 54 years old.
A Diagnosis Delayed, A Life Upended
Mison's story began in 2007 when her mother started showing cognitive issues. Seeking help, she and her brother approached their family doctor for a referral to a neurologist. They were met with a wait time of over a year—a critical period when early intervention could have helped preserve her mother's quality of life. In desperation, they turned to the emergency room at Edmonton's Misericordia Community Hospital, only to be chastised by a doctor for seeking treatment under what was deemed "false pretenses."
This experience, Mison explains, highlights two key barriers to diagnosis. Individuals with cognitive impairment often possess a remarkable ability to mask their symptoms in front of healthcare professionals. Compounding this, many doctors lack sufficient training to recognize dementia's signs and are constrained by time, preventing thorough assessments.
Navigating a Maze of Fragmented Care
Sent home to manage delusions, psychosis, and wandering alone, the family reached a breaking point. A call to a crisis line led to a recommendation for Alberta Hospital Edmonton. There, Mison's mother was initially treated for bipolar disorder for six months. It was only after a positron emission tomography (PET) scan revealed brain atrophy that she received a definitive diagnosis: frontotemporal dementia.
In an instant, my whole life changed, Mison recounts. She became the mother to her own mother, assuming responsibility for all legal and medical decisions and embarking on the complex process of obtaining guardianship.
Her personal struggle mirrors a national crisis. Alzheimer's disease, a leading form of dementia, ranks among the top causes of death in Canada. Currently, more than 770,000 Canadians are living with dementia, a number projected to soar to one million by 2030.
A Call for Systemic Change and Recognition
Despite these staggering figures, Mison finds that navigating the healthcare system is often more traumatic than the caregiving itself. She describes dementia care as fragmented, inconsistent, and difficult, with access heavily dependent on geography, income, and local resources. Patients and their caregivers, she argues, consistently fall through the cracks of a system not designed for their needs.
Now a public relations executive and the founder of Discuss Dementia, an advocacy group, Mison uses her voice to promote public discussion and policy change. Her 19-year journey is more than a personal story; it is a powerful call to action. She urges for greater recognition of dementia's impact, improved training for healthcare providers, reduced diagnostic wait times, and the creation of a coherent, supportive care system that upholds the dignity of those living with the disease and the families who stand by them.
As the population ages, the urgency for a coordinated national strategy on dementia has never been clearer. Stories like Mison's underscore the human cost of inaction and the critical need for a healthcare response that matches the scale of this growing challenge.