The expansion of prescribing powers for pharmacists in Quebec, a move heralded as a key step to alleviate pressure on the healthcare system, is progressing slower than anticipated. Announced as a measure to improve patient access to care, the full implementation of these new responsibilities is encountering hurdles.
What Powers Were Granted?
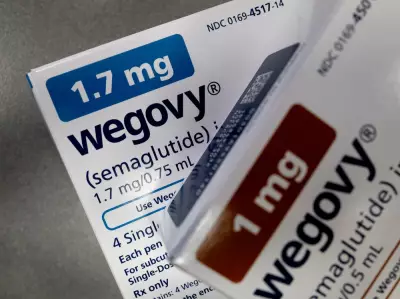
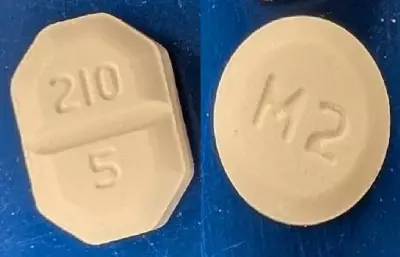
Quebec's government previously approved legislation allowing pharmacists to take on a greater role in patient care. This expansion was designed to empower them to prescribe medications for a wider range of minor ailments and to renew prescriptions for chronic conditions. The goal was straightforward: to provide patients with faster, more convenient access to essential treatments while freeing up doctors for more complex cases.
The initiative was positioned as a practical solution to long wait times and overcrowded clinics. By leveraging the widespread availability and expertise of community pharmacists, the province aimed to create a more efficient and responsive front line in healthcare delivery.
Bottlenecks in the Rollout
Despite the clear legislative intent, the translation of policy into everyday practice has been sluggish. Several factors are contributing to the delay. These include the need to finalize detailed protocols, establish clear liability frameworks, and ensure all pharmacists receive the necessary training and support to take on these enhanced duties safely and confidently.
Furthermore, integrating these new services into the provincial healthcare billing and records system requires complex technical adjustments. The coordination between the Order of Pharmacists, the government, and educational institutions is a meticulous process that cannot be rushed. This careful pace, while necessary for safety, means patients and the system are not yet realizing the full benefits promised by the reform.
Implications for Patients and the System
The delayed implementation means continued strain on traditional access points like family doctors and walk-in clinics. Patients seeking treatment for conditions like urinary tract infections, dermatitis, or needing a routine prescription renewal may still face unnecessary waits.
For the healthcare system, the holdup represents a missed opportunity to optimize resources. Pharmacists, who are highly trained healthcare professionals, remain underutilized in their capacity to provide direct care. The longer the delays persist, the longer the system foregoes a potential relief valve for its accessibility crisis.
Advocates stress that while a methodical rollout is prudent, urgency is still required. They point to other Canadian provinces where similar expansions have been successfully implemented, arguing that Quebec can and should accelerate the process to deliver tangible results to its residents sooner rather than later.