Administrative Tsunami Fuels Burnout Crisis Among Canadian Family Doctors
A growing crisis is engulfing family medicine in Canada, as physicians grapple with an overwhelming surge in administrative tasks that threatens their well-being and the sustainability of primary care. Recent data highlights a stark reality: the average family doctor now dedicates approximately nine hours each week to paperwork, emails, and bureaucratic duties—time that is increasingly seen as a primary driver of burnout.
The Rising Tide of Paperwork
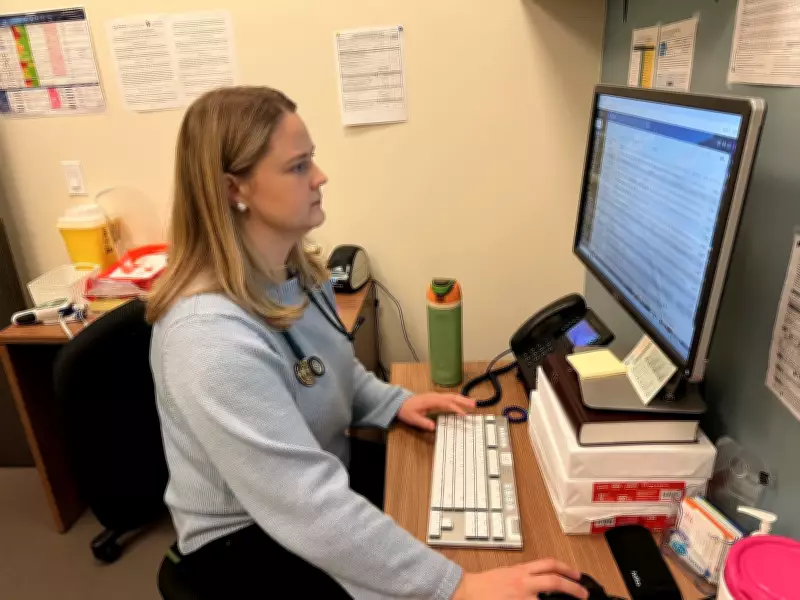
Dr. Caitlin Christie, like many of her colleagues, finds herself inundated with emails and administrative demands that detract from patient care. "It wasn't like this 20 years ago," she reflects, pointing to a dramatic shift in the daily workload of family physicians. This administrative tsunami includes managing electronic health records, navigating complex billing systems, handling insurance forms, and complying with ever-evolving regulatory requirements.
The cumulative effect is significant. What was once a manageable part of practice has ballooned into a major time sink, squeezing out opportunities for direct patient interaction and contributing to widespread exhaustion among healthcare providers.
Survey Reveals Alarming Trends
A recent survey underscores the severity of the issue, quantifying the hours doctors spend on non-clinical tasks. The nine-hour weekly average represents a substantial portion of a physician's workweek, often extending into evenings and weekends. This relentless administrative load is not merely an inconvenience; it is a critical factor in the rising rates of burnout, mental health struggles, and early retirement within the medical community.
Experts warn that this trend jeopardizes the stability of Canada's healthcare system. As family doctors reach their limits, patient access to primary care diminishes, wait times lengthen, and the continuity of care suffers. The administrative burden also discourages new graduates from entering family medicine, exacerbating existing physician shortages.
Systemic Pressures and Potential Solutions
The roots of this crisis are multifaceted. They include:
- Increased documentation requirements for legal and billing purposes.
- The proliferation of digital health tools that, while beneficial, often add layers of complexity.
- Insufficient support staff or resources to delegate administrative duties.
- A healthcare system that prioritizes procedural volume over comprehensive, relationship-based care.
Addressing this issue demands systemic changes. Potential solutions being discussed within the medical community and policy circles include:
- Investing in advanced practice nurses, physician assistants, and administrative teams to share the load.
- Streamlining billing codes and reducing redundant paperwork.
- Enhancing interoperability of electronic medical records to minimize data entry.
- Re-evaluating funding models to better compensate for the cognitive and administrative work of family medicine.
As Dr. Christie and countless other physicians navigate this challenging landscape, the call for action grows louder. Without meaningful intervention, the administrative tsunami risks washing away the very foundation of primary care in Canada, leaving both doctors and patients adrift.





